|
Written by Yoga Mamas Naturopathic Doctor Gestational diabetes (GDM) is the development of diabetes (blood sugar dysregulation) during pregnancy. It is usually diagnosed by a blood glucose challenge test between 24-28 weeks of gestation. It is important to prevent GDM because it can cause complications for mama and baby like pre-eclampsia and predisposition to diabetes after birth. The good news is, there is a lot that can be done to prevent and manage GDM to reduce the severity and risks for mama and baby! GDM is a complex disease with several contributing factors, including a disruption in glucose and lipid metabolism, inflammation and changes in the gut health. Yoga Mamas Naturopathic Doctor, lists 5 tips to help prevent and manage gestational diabetes. 1) Walk for at least 10 mins, 30 mins after every meal Moderate-intensity walking after meals can reduce post-meal blood sugar spikes and improve overall blood glucose control in women with GDM. Some studies show that walking 30 minutes after meals may be the optimal time frame in order to optimally modify the glycemic (blood sugar) response. Timing your walks in this way may have a greater positive influence on GDM than simply walking for 30 minutes per day at a non-specific time. 2) Eat complex carbohydrates high in fiber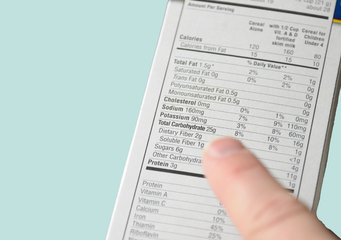 Prenatal mamas should aim for 25-30g of fibre/day in pregnancy. Unlike simpler carbohydrates (ie white bread), healthier complex carbohydrate options provide the body with essential fibre which is digested more slowly in the gastrointestinal tract and doesn’t get directly converted into sugar. These two factors explain why complex carbohydrates produce less significant post-meal blood sugar spikes and may lead to reductions in insulin resistance (an important factor in the development of GDM). Fibre also lowers the risk of obesity, heart disease and inflammatory illnesses. The fibre content of food items can be found listed under the carbohydrate section in the nutritional breakdown. Higher fibre contents reduce the total amount of carbohydrate that gets converted directly into sugar. For example, a food item with 20g of total carbohydrates and 2g of fibre is a poorer option for blood sugar control than a food item with 20g of total carbohydrates with 15g being from fibre. Downloading a Glycemic Index (GI) food guide may help you choose healthier carbohydrate options. You may download A Glycemic Index Food Guide, here: https://guidelines.diabetes.ca/docs/patient-resources/glycemic-index-food-guide.pdf 3) Eat smaller and more frequent meals throughout the day, spreading daily total carbohydrate intake over 5-7 small meals The Endocrine Society recommends limiting total carbohydrate intake to 35-45% of total calories/day for women with GDM. (Caloric needs differ amongst individuals but in general, it is recommended that pregnant women consume about 1,800 calories/day in first trimester, 2,200 in second trimester and around 2,400 calories/day in third trimester. Proper nutrition, however, should be based on consuming well-balanced meals and eating whole foods as much as possible, rather than focussing on counting calories.) The amount of carbohydrates eaten at one time can proportionately raise blood sugar higher. Therefore, the American College of Obstetrics and Gynecologists recommends spacing your meals and carbohydrates out throughout the day, consuming three smaller meals and 2-4 snacks per day. Eating regularly and consuming smaller meals may help to decrease blood sugar spikes and improve glucose control in women with and without GDM. Eating smaller and more regular meals may also help to reduce nausea, dizziness, shakiness and other unpleasant pregnancy symptoms. 4) Pair carbohydrates with protein or healthy fats but limit saturated fatsProtein requirements naturally increase in pregnancy. Eating adequate amounts of protein in pregnancy can also help to offset nausea and vomiting of pregnancy, too! Since protein and fats take much longer to digest than carbohydrates they can keep you full longer throughout the day and offset spikes in blood sugar. This is why I always recommend that snacks consisting of carbohydrates be paired with a protein or healthy fat. For example, an apple with a handful of nuts and seeds or a whole grain piece of toast with avocado. When consuming fats, saturated fats should be avoided, especially for women with GDM. A high intake of saturated fats can interfere with insulin signalling and can increase inflammation and endothelial dysfunction which are both contributing factors in GDM. On the flip side, healthy fats, such as those derived from fish, seafood, some nuts and seeds can have anti-inflammatory properties and are associated with a reduced risk of GDM. 5) Eat a snack before bed
Need more healthy lifestyle advice? Book a consultation with a Yoga Mamas Naturopathic Doctor.
A Naturopathic Doctor can help with:
REFERENCES:
https://pubmed.ncbi.nlm.nih.gov/29272606/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267507/ https://link.springer.com/article/10.1007/s00125-016-4085-2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7071246/ https://yalehealth.yale.edu/gestational-diabetes-treatment-plan https://www.karger.com/Article/Fulltext/486810#:~:text=Multiple%20studies%20have%20reported%20that,levels%20%5B14%2C%2015%5D https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-020-00509-0 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6823013/ https://pubmed.ncbi.nlm.nih.gov/28927313/#:~:text=Conclusions%3A%20Compared%20with%20control%20intervention,gestational%20age%20and%20gestational%20weight https://www.nature.com/articles/s41598-020-74773-8 https://www.cdc.gov/diabetes/basics/gestational.html#:~:text=However%2C%20about%2050%25%20of%20women,your%20levels%20are%20on%20target Posture Check! Maintaining a healthy posture during pregnancy is important to help keep mama and baby healthy. Proper posture can decrease neck, mid-back, low back, pelvic, and feet pain. These guidelines will help you maintain a healthy posture throughout your pregnancy when standing, sitting and lying down.
Lying Down Lying on your side is a recommended position to take off tension from the lower back. During the third trimester, it is not recommended for pregnant women to lie on their back for long periods of time. The weight of the baby can press on large blood vessels and reduce blood flow to the placenta and baby.
Good posture can make you look and feel better, as well as help you avoid some of the discomforts that can occur later in pregnancy.
Have you been experiencing constipation, nausea, or heartburn since becoming pregnant? During pregnancy mamas often experience digestive issues. Thankfully, there are ways to mitigate a troubled tummy. We spoke to a Yoga Mamas' Holistic Nutritionist, who listed 6 of their go-to tips:
There are so many options out there for prenatal vitamins, all the choices can be overwhelming! Prenatal vitamins help keep you and your baby healthy. It’s recommended that you take prenatal vitamins 3 months prior to trying to conceive, for the duration of your pregnancy and three months postpartum to help you recover. Taking prenatal vitamins while you’re pumping or breast/chestfeeding is also recommended. Yoga Mamas' Naturopathic Doctor, Dr. Shannon Vander Doelen made a short list of things she recommends her clients to be mindful of when making the decision. Below are three things to consider when choosing a prenatal:
Speak with your health practitioner when deciding on which prenatal vitamin to take. If you’re looking for a naturopathic doctor, Dr. Shannon Vander Doelen is accepting new patients! She’s available online and can treat anyone who resides in Ontario. Meet Dr. Shannnon Vander Doelen, Naturopathic Doctor
|
Categories
All
Archives
July 2024
|
-
Wellness Services
- Wellness Concierge
- Abdominal Massage
- Acupuncture
- Cosmetic Acupuncture
- Cesarean Scar Release Therapy
- Chinese Herbal Medicine
- Chiropractic Care
- Counselling >
- Craniosacral Therapy
- Online EFT Tapping
- Fascial Stretch Therapy
- Home Visits
- Online Holistic Nutrition
- Gua Sha Glow Facial
- Introduction to Solids
- Infant & Kids Massage
- Infant Sleep Consulting
- Kinesiology
- Kinesio Taping
- Lactation Consulting
- Light Therapy >
- Lymphatic Drainage Massage
- Massage Therapy
- Naturopathic Medicine
- Osteopathy
- Pelvic Floor Physiotherapy
- Physiotherapy
- Pediatric Physiotherapy
- Online Speech Language Therapy
- Ultrasound For Blocked Ducts
- Vitamin Injections
- FITNESS
- Doula Care
- WORKSHOPS & EVENTS
- Free Events
- Professional Trainings
- Blog
- SHOP ONLINE
Services |
ABOUT US |
|
A Note About yoga Mamas' Cancellation Policies
Please note that we do not offer refunds. Each event/course/training/wellness appt has it's own specific cancellation policy which is listed on each registration page. Please take the time to read these in full prior to registering. Each event/appointment that we run is in partnership with a practitioner who is focusing their independent career in prenatal and postpartum health. This is their beautiful livelihood. This is why we have these policies in place. Thank you very much for your understanding. Jamie Kalynuik, Founder of Yoga Mamas
[email protected] | 416-406-0116 | 1402 Queen St E Suite D. Toronto M4L 1C9
-
Wellness Services
- Wellness Concierge
- Abdominal Massage
- Acupuncture
- Cosmetic Acupuncture
- Cesarean Scar Release Therapy
- Chinese Herbal Medicine
- Chiropractic Care
- Counselling >
- Craniosacral Therapy
- Online EFT Tapping
- Fascial Stretch Therapy
- Home Visits
- Online Holistic Nutrition
- Gua Sha Glow Facial
- Introduction to Solids
- Infant & Kids Massage
- Infant Sleep Consulting
- Kinesiology
- Kinesio Taping
- Lactation Consulting
- Light Therapy >
- Lymphatic Drainage Massage
- Massage Therapy
- Naturopathic Medicine
- Osteopathy
- Pelvic Floor Physiotherapy
- Physiotherapy
- Pediatric Physiotherapy
- Online Speech Language Therapy
- Ultrasound For Blocked Ducts
- Vitamin Injections
- FITNESS
- Doula Care
- WORKSHOPS & EVENTS
- Free Events
- Professional Trainings
- Blog
- SHOP ONLINE